Presentation: Head-to-Head Comparison of 18F-Fluciclovine and 68Ga-PSMA-11 in Prostate Cancer
Drs Steven Finkelstein and Louis J. Mazzarelli highlight data revealed in the article “A Prospective Head-to-Head Comparison of 18F-Fluciclovine With 68Ga-PSMA-11 in Biochemical Recurrence of Prostate Cancer in PET/CT,” by Birgit Pernthaler, et al.
Episodes in this series
Steven Finkelstein, MD, DABR, FACRO: Let’s get into some of the details of the paper. If we look first at the patient characteristics on this study. There were 58 patients with biochemical recurrence of prostate cancer after a definitive primary therapy. What’s that? That’s either surgery or radiation therapy. And both scans were performed within a mean interval of 9.4 days. There wasn’t a great stretch where some new development, some new metastasis, was probably going to happen. A very short interval between the 2 scans. All scans were visualized and analyzed independently on a patient, on a region, and on a lesion-based analysis. All exams were performed in the same medical department using identical scanners. It wasn’t like this place had this kind of scanner [and another place] had a different kind of scanner. The scanners are the same, and the people looking at it are the same. What changed is the 2 different modalities. Louis, do you want to walk through the patient characteristic slide a little?
Louis J. Mazzarelli, MD: One thing that you first have to look at when you look at this paper is that we weren’t dealing with a population that was stratified to a very low PSA [prostate-specific antigen]. This was a wide range of PSA, both at diagnosis and at the time of scan importantly. You had PSAs that varied from a very low 0.2 ng/mL to 230.4 ng/mL. That’s incredibly important from a perspective of understanding the data. We’re not localizing to a very low PSA.
The other thing that’s interesting is that we have a range of Gleason scores. Among those included were 4 patients who at the time of diagnosis had Gleason 3 disease, which is interesting that they went on to definitive therapy. That’s something that wasn’t clarified in the paper that I’d like to learn a little more about. Otherwise, we have patients who have a Gleason score anywhere from 7 to 10, so presumptively had clinically significant prostate carcinoma.
We had no patients who had metastatic disease. We had patients who at the time of diagnosis had nodal disease, but none who had disease within the bones. That’s important. The other thing that’s important is that, as you mentioned, there’s a difference in how these were treated. The majority of patients were treated with radical prostatectomy and a smaller number of patients were treated with radiation therapy.
Steven Finkelstein, MD, DABR, FACRO: That’s excellent. When I look at some of the patient characteristics, I echo your comments. When you look, typically people are going to present in the recurrent setting or with more advanced disease. There are very few patients who by their Gleason score would be thought of as low risk: classic D’Amico low risk or NCCN [National Comprehensive Cancer Network] low or very low risk. Most of the patients would be felt to be favorable, unfavorable, intermediate risk, or higher. However, some of the nuances you alluded to are still not known. When we look, this group of patients represents that 72% of the patients underwent radical prostatectomy, whereas only 28% underwent radiation therapy.
We know that from the American Cancer Society data that with older men, the overwhelming choice of therapy is radiation therapy at a 3:1 ratio. This doesn’t represent exactly what we’re seeing from a patient characteristics perspective with older men or people with recurrence. This is unique to their experience in Europe.
Let’s go on and talk about localization of positive lesions. Louis, do you want to kick us off about what we’re talking about and how they broke up where a recurrence might be?
Louis J. Mazzarelli, MD: They decided to determine where they were based on the 4 regional areas that you would think of when you think about recurrence. Of course, you’d think about disease locally in the prostate or prostate bed. Of course, it’s a prostatectomy, so we’re thinking about the prostate bed. If it’s local pelvic disease, so not nodes outside the pelvis. If it’s extrapelvic disease, extending in the other known target regions for disease, the retroperitoneum. And then of course the bone. Not viscera but the bone. In terms of positivity, in terms of localization, what they identified was that a greater number of patients were identified with 18F-fluciclovine at the bed compared with gallium PSMA [68Ga-PSMA-11]. But when we looked at other sites of disease, the pelvis itself, extrapelvic lymph nodes, and bone metastatic disease, gallium-68 demonstrated a higher percentage of positivity. That being said, when we look at the P values, the most significant P value would be at the local bed, where 18F-fluciclovine in the context of this study did better at the local bed than PSMA [prostate-specific membrane antigen]. The numbers otherwise were close. They weren’t necessarily significant but did favor 68Ga-PSMA-11.
Steven Finkelstein, MD, DABR, FACRO: Perfect. I echo your comments about the previous slide. When we look at the number of patients who had radiation therapy, it’s only 1 of 4. When you’re looking at a local recurrence in the prostate, most patients don’t have prostates to recur. It does affect how we’re looking at the data set a little. Irrespective of that, when we look at local recurrence—i.e., in the postprostatectomy area, which represents over 75% of patients—you’re looking that there was more detection using Axumin [18F-fluciclovine] than there was for the PSMA scans. Why is that? This gets into some of the nuances of reading the scans. Louis, do you want to talk a little about when you’re looking locally in the bed vs looking for distant disease? What are some of the nuances—based on what happens in technique—that can throw off your ability to read?
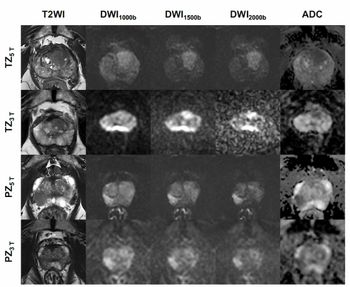
Louis J. Mazzarelli, MD: That’s the crux of the argument in this paper. Let’s talk little about physiology: 18F-fluciclovine vs PSMA. If you have that image up, it helps to illustrate it a little. First and foremost, we talk about urine excretion. When we talk about PSMA agents, they’re genitourinary excreted. Therefore the amount of radiotracer that you’re going to find in the kidneys and the bladder is going to be greater than you will with 18F-fluciclovine. As an aside, I want to comment about uptake in other places. As I mentioned, there’s going to be more background marrow uptake with 18F-fluciclovine compared with PSMA agents. There’s going to be more uptake in muscle with 18F-fluciclovine than there’s going to be with PSMA agents.
What’s crucial is technique. When we look at the technique, and we’ll talk a little about this in the papers, how did [Birgit] Pernthaler do this, in terms of gallium-68 vs 18F-fluciclovine? Typically, when we do an 18F-fluciclovine study, we acquire those images approximately 4 to 5 minutes status post-injection of radiotracer. We’ll begin an acquisition from the thighs and head to the vertex. That’s your standard 18F-fluciclovine acquisition. What’s interesting is that there’s a debate about how to acquire PSMA or 68Ga-PSMA-11, or 18F-fluciclovine. How do you do that? In the Pernthaler article, they did dynamic images initially through the pelvis, which were about 5 or 6 minutes. Then they went back at 60 minutes and did an acquisition from the vertex to the thighs. They didn’t start from the thighs to the vertex, and I say that only because over the acquisition time you’re going to be accruing more radiotracer within the bladder. Many sites, and this is just anecdotal, will start from below and then head above.
The other thing that wasn’t done in the Pernthaler article, which some places do, was acquiring delayed images through the pelvis with high resolution. In other words they’ll acquire the images over a longer bed time. Interestingly, on the 18F-fluciclovine side, the number of minutes of bed acquisition for the prostate was 5 minutes for 2 beds within the pelvis. For the 68Ga-PSMA-11 agent, it was 2.5 minutes through the pelvis, so there was a difference in acquisition. Those things are crucially important.
Just as an aside, when you interpret the images, 1 thing that’s crucially important—and it’s pointed out on this slide—is that this is an example of a patient who had a recurrence that was identified with 18F-fluciclovine but not with PSMA. Why was that the case? In this case, we can see that here’s the standard grayscale imaging. This is the low-dose noncontrast CT scan. Here’s the PET [positron emission tomography] without the fusion, and of course we have the fusion images. What’s happened is that the bladder is obscuring the uptake within the region of concern or disease recurrence within the prostate. This is the crux of where a difference in local recurrence may occur. I’ll make some more comments, but what are your thoughts when you look at these images? [How are you] feeling about the way the images look?
Steven Finkelstein, MD, DABR, FACRO: The hardest area for us is around the bladder. They asked Willie Sutton once, “Why do you rob banks?” He said, “That’s where the money is.” Where the prostate was is probably the area with highest risk of recurrence. That’s why postprostatectomy radiation therapy has been so successful. When the RTOG [Radiation Therapy Oncology Group] put together a consensus about what to aim at, we created what’s called an RTOG atlas consensus statement—here’s where we need to aim. That was the area where the prostate was and into the bladder a little. That would represent what we’re seeing here: 1 of 6 patients with a positive local recurrence on Axumin [18F-fluciclovine] that wasn’t demonstrated on a 68Ga-PSMA-11 scan. Why? Because the bladder uptake obscures your ability to detect it.
In the old days, before we had this fancy next-generation imaging, we’d cover where we thought the prostate cancer occurrences could be based on historical data and historical information. We were somewhere between 40% and 70% of the time, but it would be much better to be able to target areas of specific recurrence. Then we were doing Axumin [18F-fluciclovine] scans, able to find where these sites of recurrence were. Some of them in the areas of the seminal vesicles remnants, some near the area of where the anastomosis was, but in general we were finally able to see where these areas of occurrences were and how that could potentially lead to improvements in outcome. In fact, EMPIRE-1 was a trial that looked to see if imaging could be a relevant biomarker to drive care and show that an improvement in care using next-generation imaging to guide radiation therapy in those patients. It’s obviously very exciting. PSMA unfortunately has its issues with being obscured by the bladder uptake. From my standpoint as a radiation oncologist, if it’s obscured and the radiologist or the nuclear medicine physician doesn’t read that there’s disease there, that could cause the patient to not have the best outcome with respect to getting the right next therapy.
As we go into the next slide, we’re going to see something that’s remarkable for PSMA imaging agents, which is the ability to detect bone metastases. Louis, talk me through a little about how you think the 18F-fluciclovine and PSMA agents have done from your experience and from this trial?
Louis J. Mazzarelli, MD: One thing you know when you look at the fused images and when you look at the PET-only images is the uptake that’s a baseline uptake within bone. When we look at this vertebra and the uptake in the bone, we see that there’s clearly some uptake within the marrow; therefore, that could easily obscure the identification of a small or not particularly avid metastatic focus. Whereas when we look at the PSMA study, we see a large difference in terms of the amount of uptake within bone. Clearly, when the background is very low, the ability to identify a lesion is going to be easier and become more overt.
One comment that you can make about 18F-fluciclovine before we had PSMA was that we did note that lesions that were particularly sclerotic could be very difficult to see and distinguish as being neoplastic. Anecdotally, in my experience with PSMA, the background of uptake in the marrow is so low. Perhaps 1 of many reasons why PSMA outperforms 18F-fluciclovine within the skeletal system is the absence of background uptake. That will make a huge difference.
There are other things that are at play, and we’ll talk about those. Sometimes, simply, it’s about density. With PET, we’re all about resolution. How small can something be identified as positive is dependent on the concentration of radiotracer within it. If something is on a micromolecular level, we’re not going to see it regardless of how good our radiotracer is because it doesn’t have enough resolution. But even very small lesions, because the density of PSMA is so high within these lesions, we can identify these very small lesions. In this case perhaps 18F-fluciclovine because it’s a different mechanism of an action, it’s an amino acid transporter, it doesn’t have the density of uptake to be shown as being positive outside the issue of background. Those are the 2 comments I would make when I look at this comparison.
Steven Finkelstein, MD, DABR, FACRO: That’s perfect. When we talk about this for the radiation oncologist looking at these images, unfortunately we’re seeing that where there’s probably a lesion, their PSMA is detecting that lesion but 18F-fluciclovine did not within a distant site of metastasis. With that, we’re getting better visualization of smaller amounts of disease using a PSMA-imaging agent.
Louis J. Mazzarelli, MD: Yes.
Steven Finkelstein, MD, DABR, FACRO: What about lymph nodes? Our next image is a set of positive lymph node metastasis looking at 18F-fluciclovine on the top and 68Ga-PSMA-11 on the bottom. Both modalities are detecting the lymph nodes, but you can see a much more robust pattern. I’ll let Louis as the imager give a little more nuanced comment to it.
Louis J. Mazzarelli, MD: Here you get a good sense of it, just to talk about physiological uptake. Both radiotracers have physiological uptake within the liver, and you can see radiotracer uptake within the kidneys but notice the difference in the PSMA study of the kidneys compared with the 18F-fluciclovine study. Here we have negative uptake within a renal cyst. But we have positive nodes, which are in the retroperitoneum and are clearly more identifiable and more scintigraphically evident on the PSMA study. We have to wonder why that is. We have to look at the mechanism of the radiotracer and understand that perhaps it’s because of the density of radiotracer being accumulated. In other words, does this tumor that has metastasized the retroperitoneum have a higher concentration of PSMA on its surface, which is allowing the radiotracer to outperform the 18F-fluciclovine? Regardless of the ability of the 18F-fluciclovine to identify the nodes, it’s a matter of concentration of radiotracer based on the molecular behavior of the tumor. In general, we’ve seen that largely be the case, that nodes—especially extrapelvic nodes—are better identified with PSMA than they are with 18F-fluciclovine. But that’s not entirely the case. As you see from some of the data within this paper, there are cases where 18F-fluciclovine outperformed PSMA on individual patients within the nodal beds, which is an interesting commentary on disease heterogeneity; that’s interpatient heterogeneity. There’s a lot going on.
Steven Finkelstein, MD, DABR, FACRO: Let’s get a into some of the specific data of the study. When we talk about detection of local recurrence and metastasis, the first thing is the overall detection rate for prostate cancer recurrence in this study: 79.3% in the 18F-fluciclovine arm and 82.8% in the 68Ga-PSMA-11 arm. Local recurrence was detected in 37.9% of patients on the 18F-fluciclovine arm and 27.6% on the 68Ga-PSMA-11 arm. Local pelvic lymph node recurrence was detected in the 18F-fluciclovine arm vs the 68Ga-PSMA-11 arm in 46.6% of patients vs 50%, and in extrapelvic lymph node metastasis in 41.4% vs 51.7%. Finally, when we look at bone metastasis, we’re looking at 25.9% vs 36.2%. Louis, walk us through this slide, which shows it in graphical form. It shows us issues with respect to 1 study, the other study, both, or none.
Louis J. Mazzarelli, MD: We get back to the idea of local recurrence to start. First, we see that there were no patients where local recurrence was identified only by PSMA and not by 18F-fluciclovine, but the converse was true where 18F-fluciclovine was able to identify a local recurrence and PSMA could not. When we look at the other sites of disease—the pelvic lymph nodes, the extrapelvic spaces, within the bone—we see that there are patients for whom only PSMA could identify the disease within the pelvic nodes, within the bones, and within the extrapelvic lymph nodes. That gets you to the large conclusions we’ve made, which is that the radiotracers perform very admirably. They perform admirably, but PSMA outperformed 18F-fluciclovine when it came to spaces outside the local bed. In this case, the local bed favored 18F-fluciclovine in terms of the ability to identify disease.
Transcript edited for clarity.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.