Utilizing PSMA-PET Scan to Detect Prostate Cancer
Experts highlight the use of PSMA PET scans as a recent and accurate imaging method for prostate cancer screening.
Episodes in this series

Umesh D. Oza, MD: Let’s focus and shift our attention to what has obviously changed. Your and my practice, along with many radiologists, urologists, [and] oncologists, has changed the landscape for our patients. It’s PSMA [prostate-specific membrane antigen] PET-CT. Could you please give a general introduction to PSMA PET, discuss its advantages as a modality compared to traditional CT and bone scans? Essentially, how has this new modality, or, rather, this new tracer for the modality we’ve been using, come about?
Jaideep S. Sohi, MD: Absolutely, a wonderful and talkable question. We’ve been using PET-CT imaging for almost 30 plus years in clinical scenarios. As you mentioned earlier, Dr Oza, we do have F 18 FDG [fludeoxyglucose F 18] PET that has limited utility in prostate cancer due to its low uptake. Now we have a new tracer, PSMA PET. PSMA stands for prostate-specific membrane antigen. It’s a transmembrane enzyme that is overexpressed by a large factor in nonprostate cancer cells. So we now have a modality that, although not 100% specific for prostate cancer, is much more specific than F 18 FDG, which we’ve used in the past. This tracer allows for more accurate visualization of prostate cancer lesions. PSMA PET has been used in Australia and Europe for over 7 years and has recently become available in the US. What are your thoughts on this?
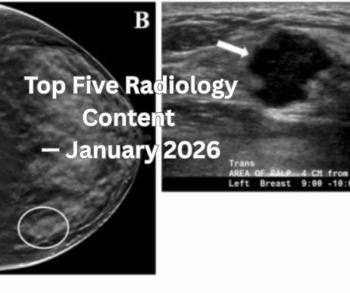
Umesh D. Oza, MD: Absolutely, I agree with you. In simple terms, it’s a game changer. We’re no longer [uncertain] about diagnoses or what we’re seeing. We’re now able to clearly identify these very bright lesions, as we discussed earlier, even small lesions in the periprosthetic area, deep pelvic nodal stations, and perirectal nodal stations that we might have previously dismissed as vessels or something minor. We can now confidently identify positive disease. At the same time, when we see these bright lesions with standardized uptake values in the 10s, 20s, and sometimes even higher, we can trust that a negative PSMA PET scan truly indicates no metastatic disease, locally or distantly. This is a significant improvement compared to F 18 FDG, which we used to consider less sensitive and specific, often requiring continued follow-up. So it has indeed changed the landscape of what we’re doing.
Jaideep S. Sohi, MD: One thing to remember is that we’ve mentioned earlier the limitations of conventional imaging, CT and bone scan. Here we have now this modality where it basically takes the best of anatomic and metabolic imaging and fuses them together. So we’re able to look at the whole body from proximal, midthighs to skull vortex and look at soft tissues and bony structures. We’re able to resolve the challenges that we have encountered with CT and bone scan. In other words, like you said, small lymph nodes are 2, 3, 4, 5 mm in size, depending on the camera and resolution and reconstruction techniques. And I’m able to resolve small lymph nodes, which are not often enlarged in prostate cancer.
Transcript is AI-generated and edited for clarity and readability.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.