Multislice CT bolsters coronary plaque analysis
Acute coronary syndromes, especially acute myocardial infarction and sudden cardiac death, are most often caused by the rupture or erosion of coronary atherosclerotic plaques. The plaque itself does not have to be associated with lumen narrowing.
Acute coronary syndromes, especially acute myocardial infarction and sudden cardiac death, are most often caused by the rupture or erosion of coronary atherosclerotic plaques.1 The plaque itself does not have to be associated with lumen narrowing. Coronary blood flow may be obstructed by a thrombus forming at the site of plaque rupture. In fact, the majority of lesions that cause acute coronary syndromes are not stenotic before the event occurs.
Patients are frequently entirely asymptomatic up to their first coronary artery disease event, which may be sudden death. Identification of patients at risk of acute coronary syndromes is consequently difficult. Atherosclerotic risk factors such as hypertension, family history, diabetes, elevated cholesterol, and smoking have been used to identify patients at risk, but their predictive accuracy is limited.
The continuous improvement of invasive and noninvasive imaging technology has made it possible to visualize coronary atherosclerotic plaques directly. Imaging-led detection, quantification, and characterization of coronary atherosclerotic plaque may potentially be an accurate way of detecting high-risk patients requiring pharmacological intervention. Imaging may also be able to single out individual atherosclerotic plaques that pose a very high risk (vulnerable plaques) and may be amenable to local treatment.
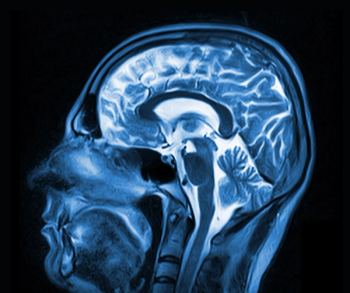
Invasive methods for visualizing coronary atherosclerotic plaque include intravascular ultrasound, optical coherence tomography, and angioscopy (Figure 1). Their invasiveness and high cost and the potential risk of complications should restrict these methods to selected patient groups. MRI has demonstrated its potential to visualize, quantify, and characterize atherosclerotic plaque in some of the larger arteries, such as the aorta and carotids. Limited spatial resolution, however, makes coronary MRI extremely challenging, and the modality is currently unable to visualize coronary artery plaque reliably.2
Limited spatial and temporal resolution precluded CT imaging of the coronary arteries for many years. The only exception was coronary artery calcification assessment (Figure 2) using electron-beam CT. EBCT scanners were designed specifically for cardiac imaging, providing a temporal resolution of 100 msec. The presence and amount of coronary calcification, as assessed by EBCT, has been shown to be a very strong predictor of future cardiovascular disease events.3
PLAQUE VULNERABILITY
Several prospective studies have also demonstrated convincing evidence that coronary calcium has stronger predictive power than the assessment of cardiovascular risk factors. Not all coronary atherosclerotic plaques contain calcium, though, and the extent of calcification is not related to plaque stability or vulnerability. EBCT's relatively low spatial resolution and high image noise make the modality unsuitable for reliable assessment of noncalcified plaque components.
The introduction of multislice CT scanners offering considerably better temporal resolution than early-generation spiral CT technology has made it possible to perform cardiac CT. The coronary arteries can be visualized reliably with 16- and especially 64-slice CT, given certain prerequisites: Patients need to have a regular and preferably low heart rate (below 65 bpm), they should not be too obese, and they need to cope with breath-hold acquisitions of approximately 10 to 20 seconds duration.
The initial focus of coronary imaging using 16- and 64-slice CT has been contrast-enhanced detection of coronary artery stenoses. This proved to be reasonably accurate with sufficient image quality. Initial investigators also recognized the potential of MSCT to visualize coronary atherosclerotic lesions in these contrast-enhanced scans, whether or not they were associated with significant stenosis.4,5 MSCT can detect calcified and noncalcified plaque components (Figure 3). The potential of this information for risk stratification has sparked intense interest in plaque imaging to identify patients at high risk of a coronary event.
PLAQUE DETECTION
Several studies have evaluated the accuracy of 16- and 64-slice CT to detect the presence of nonstenotic coronary atherosclerotic plaque. These investigations validated MSCT against intracoronary ultrasound and assessed the ability of MSCT to detect plaque in certain coronary artery segments. Detection of single coronary plaques was not considered.
Schoenhagen et al reported an accuracy of 80% for the detection of noncalcified plaque with 16-slice CT.6 Achenbach et al found a sensitivity of 82% and specificity of 88% in 22 patients, though this high sensitivity was driven by the detection of calcified plaque. Segments with entirely noncalcified plaque were identified with a sensitivity of only 53%.7 Leber et al reported a sensitivity and specificity of 84% and 91%, respectively, for the detection of nonobstructive plaque by 16-slice CT in comparison to intravascular ultrasound.8 This same group also studied 19 patients on 64-slice CT and found sensitivities of 83% for the detection of noncalcified plaque, 94% for the detection of mixed plaque, and 95% for the detection of calcified plaque. Specificity was 95%.9
Van Mieghem et al demonstrated the influence of plaque size on sensitivity using 64-slice CT. They reported 76% sensitivity for the detection of lesions greater than 2 mm and 60% sensitivity for lesions smaller than 1 mm. Overall, MSCT yielded a sensitivity of 86% in this analysis of 67 coronary arteries and a specificity of 69%.10
The reported accuracies certainly sound impressive. It is important to note, however, that these results were obtained by experienced investigators in selected groups of patients, all of whom had coronary vessels large enough for study by the relatively bulky intravascular ultrasound catheters used as a reference standard. The true accuracy of MSCT in everyday scans is difficult to assess, but it is likely to be lower than that reported in the scientific studies. For example, motion artifacts mimicking the appearance of noncalcified plaque can lead to false-positive diagnoses. On the other hand, improvements in CT technology, such as the introduction of dual-source scanners, should make plaque detection more reliable in the future.11
CHALLENGING MEASURES
The small size of coronary arteries means that CT-based plaque measurements are challenging. Moselewski et al found a relatively poor correlation coefficient of r2 = 0.55 for the measurement of cross-sectional areas of noncalcified coronary plaque by 16-slice MSCT compared with intravascular ultrasound.12
For plaque volumes, Achenbach et al reported a moderately high correlation coefficient of r2 = 0.8 when comparing plaque volume per coronary segment between 16-slice MSCT and intravascular ultrasound.7 In a study performed using 64-slice CT, Leber et al found a significant and moderately close correlation for plaque volumes per 3-mm coronary artery section, with a correlation coefficient of r2 = 0.83. But CT significantly underestimated plaque burden in this study. The mean interobserver variability for measuring plaque volumes was 37%, illustrating the difficulty of measuring these tiny structures with CT.9
Several factors are assumed to influence the vulnerability of a coronary atherosclerotic plaque. These include macrophage content and the thickness of the protective fibrous cap. Fibrous caps thinner than 65 micron are assumed to imply increased risk of plaque rupture, but dimensions in this range cannot be measured by coronary CT.
The lipid content of atherosclerotic lesions is also believed to be associated with their risk of rupturing. Several investigators have explored the ability of MSCT to differentiate lipid-rich from fibrous lesions by measuring CT attenuation values within the plaque. It has consistently been shown that plaques with a lipid-rich appearance on intravascular ultrasound have lower CT attenuation values than plaques with a fibrous appearance (see table).13-18
CT attenuation values vary widely from one study to the next, however. Significant variation is also observed within plaques of a similar type in the same study.18 So while mean attenuation values may differ between plaque types in a large sample, characterization of a single plaque based on measured CT attenuation alone does not seem possible. It has additionally been shown that external factors, such as contrast concentration in the coronary artery lumen, have a strong influence on CT attenuation values measured within coronary atherosclerotic plaques.19,20 This further complicates CT-based plaque characterization. The necessary standardization of acquisition parameters will be extremely difficult to achieve.
CLINICAL SIGNIFICANCE
Despite the tremendous wealth of data on the prognostic significance of coronary calcium, information on the clinical meaning of noncalcified, nonobstructive plaque detected by CT is not available. Three retrospective studies in small patient groups (23 to 42 patients) have shown that noncalcified plaque is more prevalent in patients with acute coronary syndromes than in patients with stable coronary artery disease.21-23
No prospective trials have been conducted yet, and the predictive power of noncalcified plaque regarding the occurrence of future cardiac events is unknown. Noncalcified plaques are, in fact, detected frequently in contrast-enhanced data sets acquired for coronary CT angiography.24 It would be easy to assume that an individual whose CT data show the presence of noncalcified coronary plaque is at an increased risk for future coronary events. Yet the exact meaning of this finding is not currently known. The less-than-perfect sensitivity and specificity of MSCT, especially in data sets of suboptimal image quality, also needs to be taken into account.
So what are the current clinical implications of noncalcified plaque imaging by MSCT? The relative paucity of hard data means that any conclusion-including this one-will be subject to personal opinion. It is clearly not justifiable to perform CT coronary angiography in asymptomatic individuals for the mere purpose of risk stratification. This investigation requires the use of a contrast agent and substantial exposure to ionizing radiation. The accuracy of plaque detection is also insufficient for screening purposes, and prognostic data providing guidance on the consequences of a positive scan are also unavailable.
It is much more difficult to recommend what should happen when nonobstructive plaque is detected as an incidental finding during scheduled CT coronary angiography of a symptomatic patient. The plaque's presence should probably be reported, along with a measure of confidence of this finding.
Decisions on the administration of lipid-lowering drugs must be made on a case-by-case basis, taking account of clinical circumstances. Recommendations on the management of patients with a high clinical risk profile, but no plaque detectable on CT, also cannot be taken out of their clinical context.
Prospective data on the significance of these findings are not currently available.
PROF. DR. ACHENBACH is a senior consultant in the department of internal medicine II (cardiology) at the University of Erlangen-Nuremberg in Germany.
References
- Fuster V, Badimon L, Badimon JJ, Chesebro JH. The pathogenesis of coronary artery disease and the acute coronary syndromes (I). NEJM 1992;326(4):242-250.
- Fayad ZA, Fuster V, Nikolaou K, Becker C. Computed tomography and magnetic resonance imaging for noninvasive coronary angiography and plaque imaging: current and potential future concepts. Circulation 2002;106(15):2026-2034.
- Bellasi A, Raggi P. Diagnostic and prognostic value of coronary artery calcium screening. Curr Opin Cardiol 2005;20(5):375-380.
- Schroeder S, Kopp AF, Baumbach A, et al. Noninvasive detection and evaluation of atherosclerotic coronary plaques with multislice computed tomography. J Am College Cardiol 2001;37(5):1430-1435.
- Becker CR, Knez A, Ohnesorge B, et al. Imaging of noncalcified coronary plaques using helical CT with retrospective ECG gating. AJR 2000;175(2):423-424.
- Schoenhagen P, Tuzcu EM, Stillman AE, et al. Non-invasive assessment of plaque morphology and remodeling in mildly stenotic coronary artery segments: comparison of 16-slice computed tomography and intravascular ultrasound. Coron Artery Dis 2003;14(6):459-462.
- Achenbach S, Moselewski F, Ropers D, et al. Detection of calcified and noncalcified coronary atherosclerotic plaque by contrast-enhanced, submillimeter multidetector spiral computed tomography: a segment-based comparison with intravascular ultrasound. Circulation 2004;109(1):14-17.
- Leber AW, Knez A, von Ziegler F, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am College Cardiol 2005;46(1):147-154.
- Leber AW, Becker A, Knez A, et al. Accuracy of 64-slice computed tomography to classify and quantify plaque volumes in the proximal coronary system: a comparative study using intravascular ultrasound. J Am College Cardiol 2006;47:672-677.
- Van Mieghem CA, McFadden EP, de Feyter PJ, et al. Noninvasive detection of subclinical coronary atherosclerosis coupled with assessment of changes in plaque characteristics using novel invasive imaging modalities: the Integrated Biomarker and Imaging Study (IBIS). J Am College Cardiol 2006;47(6):1134-1142.
- Achenbach S, Ropers D, Kuettner A, et al. Contrast enhanced coronary artery visualization by dual-source computed tomography - initial experience. Europ J Radiol 2006;57(3):331-335.
- Moselewski F, Ropers D, Pohle K, et al. Comparison of measurement of cross-sectional coronary atherosclerotic plaque and vessel areas by 16-slice multidetector computed tomography versus intravascular ultrasound. Am J Cardiol 2004;94(10):1294-1297.
- Estes JM, Quist WC, Lo Gerfo FW, Costello P. Noninvasive characterization of plaque morphology using helical computed tomography. J Cardiovasc Surg (Torino) 1998;39(5):527-534.
- Schroeder S, Kuettner A, Leitritz M, et al. Reliability of differentiating human coronary plaque morphology using contrast-enhanced multislice spiral computed tomography: a comparison with histology. JCAT 2004;28(4):449-454.
- Becker CR, Nikolaou K, Muders M, et al. Ex vivo coronary atherosclerotic plaque characterization with multi-detector-row CT. Europ Radiol 2003;13(9):2094-2098.
- Leber AW, Knez A, Becker A, et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am College Cardiol 2004;43(7):1241-1247.
- Carrascosa PM, Capunay CM, Garcia-Merletti P, et al. Characterization of coronary atherosclerotic plaques by multidetector computed tomography. Am J Cardiol 2006;97(5):598-602.
- Pohle K, Achenbach S, MacNeill B, et al. Characterization of noncalcified coronary atherosclerotic plaque by multi-detector row CT: Comparison to IVUS. Atherosclerosis 2007;190(1):174-180.
- Schroeder S, Flohr T, Kopp AF, et al. Accuracy of density measurements within plaques located in artificial coronary arteries by X-ray multislice CT: results of a phantom study. JCAT 2001;25(6):900-906.
- Cademartiri F, Mollet NR, Runza G, et al. Influence of intracoronary attenuation on coronary plaque measurements using multislice computed tomography: observations in an ex vivo model of coronary computed tomography angiography. Europ Radiol 2005;15(7):1426-1431.
- Leber AW, Knez A, White CW, et al. Composition of coronary atherosclerotic plaques in patients with acute myocardial infarction and stable angina pectoris determined by contrast-enhanced multislice computed tomography. Am J Cardiol 2003;91(6):714-718.
- Inoue F, Sato Y, Matsumoto N, et al. Evaluation of plaque texture by means of multislice computed tomography in patients with acute coronary syndrome and stable angina. Circ J 2004;68(9):840-844.
- Hoffmann U, Moselewski F, Nieman K, et al. Noninvasive assessment of plaque morphology and composition in culprit and stable lesions in acute coronary syndrome and stable lesions in stable angina by multidetector computed tomography. J Am College Cardiol 2006;47(8):1655-1662.
- Hausleiter J, Meyer T, Hadamitzky M, et al. Prevalence of noncalcified coronary plaques by 64-slice computed tomography in patients with an intermediate risk for significant coronary artery disease. J Am College Cardiol 2006;48(2):312-318.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.