CT overreads raise big questions about radiology's future
In this issue, legal columnist Thomas Greeson wades squarely into one of radiology's hottest topics today: cardiac CT overreads by radiologists. Under such scenarios, cardiologists interpret images of the heart and related vessels and leave the rest of the chest to radiologists. These marriages of convenience are strongly promoted in some quarters as avoiding destructive turf battles and assuring that patients get the best possible care following a chest CT scan.
In this issue, legal columnist Thomas Greeson wades squarely into one of radiology's hottest topics today: cardiac CT overreads by radiologists. Under such scenarios, cardiologists interpret images of the heart and related vessels and leave the rest of the chest to radiologists. These marriages of convenience are strongly promoted in some quarters as avoiding destructive turf battles and assuring that patients get the best possible care following a chest CT scan.
Greeson raises some pointed legal questions about the structure of these arrangements that you'll want to ponder if you're participating in such an agreement or considering doing so. But simmering just under the surface is an even bigger question that these arrangements raise: What is the future of radiology if specialists increasingly acquire their own scanners and render their own interpretations of selected organ systems, sending the rest of the data to radiologists who then review for incidental findings?
As Greeson notes in his column, "Could not orthopods seek hospital privileges to interpret MSK magnetic resonance studies in hospitals, focusing on the skeletal images and backed up by an overread of the soft tissue by radiologists?" The CCTA shared model could be extended to other procedures such as virtual colonography performed by gastroenterologists.
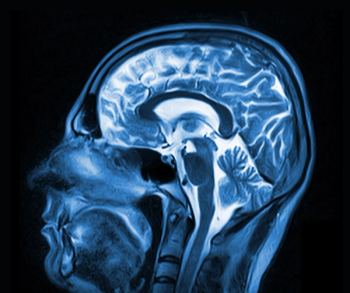
We've raised this issue before from a slightly different perspective. In our August 2005 edition, Dr. Stephen Baker, chair of radiology at the University of Medicine and Dentistry of New Jersey, lamented the prospect that vendors could design software to discard data and allow only the presentation of specific organ systems. You've all seen these images, typically featuring the 3D heart, one of which appears on our cover this month. So far such images are the products of postprocessing, but we also know that vendors are developing systems that better highlight particular organ systems.
It can be argued that neither of these trends is an immediate threat. For the most part, specialists have not moved in on primary reads of their respective organ systems. They recognize that radiologists generally have superior expertise in image interpretation.
But the experience so far with cardiology suggests that the potential for less straightforward business practices exists.
The issue becomes even more complicated when you consider how the evolution of imaging equipment will affect this process. As was the case with whole-body CT scans, today's more advanced CT devices reveal a host of new findings unrelated to the primary organ scan. A classic example concerns lung nodules that accompany cardiac CT: Should the nodules be biopsied? If they are benign, how should the increase in complications and morbidity be weighed? Specialists are already suggesting options for limiting incidental findings with tactics that include narrowing the field-of-view or using software to exclude noncardiac findings.
Certainly research will better define what constitutes an actionable incidental finding. A host of factors-reimbursement, malpractice, equipment ownership patterns, and local conditions among them-will determine how radiologists and specialists deal with reviews for primary and incidental findings. Radiologists need to watch this carefully and proceed with caution.
But eventually a consensus will emerge on the standard of care in these situations. I believe this standard of care should include the following element: Data from tissue that is irradiated should not be discarded and should be subject to review for incidental findings. Patients exposed to the risk of the scan-dose exposure and contrast nephropathy-should be entitled to an interpretation of all the data generated in that scan. There will be considerable pressure to discard this "nonrelevant data." Radiologists should resist that pressure.
What are your thoughts on this topic? Please e-mail me at
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.