Study Shows Merits of Photon-Counting CT in Detecting Subtle Post-COVID Lung Abnormalities
In a recently published prospective study comparing photon-counting detector computed tomography (PCD CT) versus energy-integrating detector CT (EID CT) in patients with persistent symptoms after COVID-19 infection, researchers found that PCD CT discovered additional lung abnormalities in half of the study participants.
For enhanced image quality and detection of subtle lung abnormalities in people who have had COVID-19 infection, emerging research suggests that photon-counting detector computed tomography (PCD CT) may be superior to conventional CT.
For the prospective study, recently published in
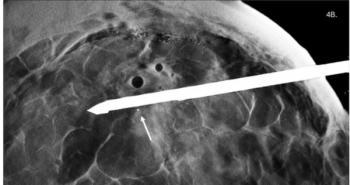
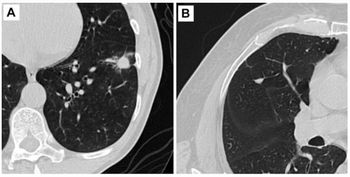
While linear bands and ground-glass opacities were the most common findings with EID CT, the researchers said PCD CT uncovered additional lung abnormalities in half of the study cohort. These findings included bronciolectasis (10 of 20 participants) and reticulations (seven of 20 participants), according to the study. The study authors added that PCD CT showed fine reticulations for six participants in areas that had been identified as ground glass opacities by EID CT.
“Photon-counting detector (PCD) CT revealed subtle lung abnormalities in symptomatic participants with persistent COVID-19 symptoms that were not detectable on energy-integrating detector (EID) CT but may be indicative of irreversible fibrosis,” wrote Benedikt H. Heidinger, M.D., who is affiliated with the Department of Biomedical Imaging and Image-Guided Therapy at the Medical University of Vienna in Austria, and colleagues.
(Editor’s note: For related articles, see “
In regard to image quality, the researchers said the reviewing radiologists found that 0.4 mm section thickness for PCD CT images was “definitely better” than 1.0 mm for all of the participants of the study. Heidinger and colleagues noted that 0.4 mm PCD CT found 17 abnormalities in nine patients in comparison to 1.0 mm PCD CT. Yet the use of 1.0 mm PCD CT in comparison to 1.0 mm EID CT revealed five abnormalities in four participants. While noting a significantly higher signal-to-noise (SNR) ratio for 1.0 mm sections of PCD CT in comparison to EID CT, the researchers said the SNR ratio was reduced for 0.2 mm and 0.4 mm sections.
“Our findings suggest that 0.4 mm sections represent a favorable compromise between ultra-high resolution and perceived (and quantitative) image quality, permitting confident detection of subtle lung abnormalities,” added Heidinger and colleagues.
Beyond the small sample size, the study authors said other possible limitations may have included slight variation between EID CT and PCD CT in the use of sharp edge-enhancing CT reconstruction kernels to help detect subtle abnormalities. They acknowledged that false positive findings on PCD CT could not be ruled out due to a lack of histopathological correlation with the study findings. The researchers added that sequential assessment of EID CT and PCD CT images may have contributed to biased views of image quality and may have prevented detection of abnormalities that were only visible on EID CT.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.