Should Radiologists Provide Reports to Patients?
CHICAGO - Patients want access to their imaging reports, but radiologists hesitate. Here’s what to consider when opening your files.
CHICAGO - Should radiologists provide reports directly to patients?
Many physicians say no. They fear that patients will be confused or stressed out by the reports. That’s not just cruel to the patient, they say, it’s also more work - we’ll spend all our time fielding calls from terrified laymen who don’t understand what they’re seeing. Really, it’s kinder to insulate them.
Patients tend to disagree.
The waiting is the hardest part
Why the disconnect? It’s possible radiologists don’t realize just how hard waiting for results can be. Annette Johnson, MD, associate professor of radiology at Wake Forest University, surveyed patients who had recently undergone scans at the facility. A whopping 92 percent of them reported they suffered from anxiety until they got their results.
So Johnson, who spoke of her survey at an RSNA 2012 session this week, gave these patients a hypothetical scenario. What if they had quick access to their results via an online portal before they talked to their doctor? She put together three scenarios. One involved a positive result - basically, nothing was wrong. One gave an indeterminate result. And one delivered very bad news in stark, medical terms.
About 80 percent of the patients Johnson talked to said they preferred to find out their results early via the portal - even the patients who got the negative diagnosis.
But that’s hypothetical, and from a small study at that. In real life, it would be different, right?
The real world
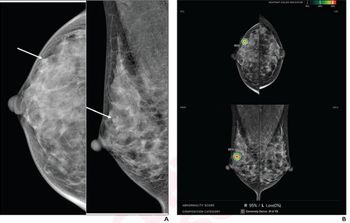
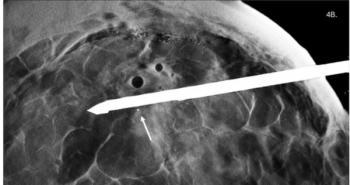
Not according to Curtis Langlotz, MD, PhD, professor of radiology and vice chair for informatics at the University of Pennsylvania. They ran a three-month pilot program allowing patients to see reports from abdominal imaging, breast imaging and interventional radiology studies via a portal.
The radiologists were nervous. Surely they’d be deluged with calls from anxious patients who didn’t understand what they were looking at.
That didn’t happen.
“We received a grand total of four patient calls, none of which were related to any of the report types that were released as a part of this project,” Langlotz said.
The results were promising enough that they expanded the program to all University of Pennsylvania hospitals in June. So far, Langlotz said, they haven’t had any problems. That’s not to say they haven’t gotten some complaints. Those complaints just tend to come from physicians.
Making it work
There are things to be aware of before you jump into sharing records. For example: Not every patient will be onboard.
“They’re all different,” Johnson said. “They don’t all want the same access. Some patients would never want to log on somewhere and see a bad result. Some of them would want to immediately regardless. They need to be able to individually choose how much access they want.”
And those who do choose to receive the reports will go over them with a fine-tooth comb, so you’d better brush up on your copyediting skills.
“We did a lot of radiologist education about this,” Langlotz said. “If a patient sees a report where it says that the gall bladder is normal, but they know that they’ve had their gall bladder out, they might assume that someone has read the wrong images, as opposed to the fact that we might have used a macro that didn’t get edited.”
If you really want to make patients happy with these sorts of reports, consider providing a layperson-friendly summary. But if that’s too much to contemplate, just providing hyperlinks to reputable information about the medical terms is almost as good.
In Johnson’s study, more than three-quarters of the patients surveyed said they’d definitely use those hyperlinks to do their own research. “They want our input on what is reliable medical information,” Johnson said.
Most of all, patients don’t want to wait. If they can get results immediately, many of them would jump at the chance - even if the news is bad.
Instant gratification isn’t always possible. But a three-day turnaround for reports would keep patients happy, give referring physicians time to review, and would fall within the federal meaningful use guidelines for electronic health records, which could put you in line for incentive payments.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.