Report from ARRS: Digital mammography systems vary widely in dose, quality
Automatic and recommended settings on digital mammography systems have a significant impact on patient dose as well as image quality, according to a study presented at the American Roentgen Ray Society meeting on Tuesday.
Automatic and recommended settings on digital mammography systems have a significant impact on patient dose as well as image quality, according to a study presented at the American Roentgen Ray Society meeting on Tuesday.
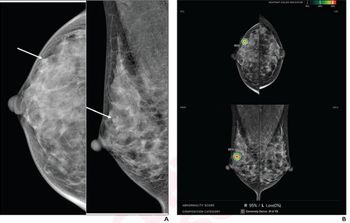
Researchers at Northwestern University found major differences in clinical quality and patient dose in images produced by four full-field digital mammography systems, said presenter Eric Berns, Ph.D., a research assistant professor at Northwestern.
All four systems studied had been approved by the FDA:
- GE 2000D
- GE DS
- Lorad Selenia
- Siemens Novation
"Our results indicate average dose varies by up to a factor of 2.6. There are also significant differences in image quality. Technique factors in automatic exposure mode selection can play an important role in image quality and patient dose," Berns said.
For all systems, researchers used the automatic and recommended settings (for example, mAs and kVp) from the manufacturer. Using phantom image techniques, they looked at average glandular dose and image quality at four levels of breast thickness: 2 cm, 4 cm, 6 cm, and 8 cm.
The researchers simulated 50% fatty and 50% glandular breasts on phantom images. They also compared American College of Radiology phantom images, which are routinely taken as part of the Mammography Quality Standards Act accreditation process, for the four scanners.
Dosage was below the recommended limit at all levels of breast thickness for all four scanners, but differences appeared that were statistically significant. At the lowest level of breast thickness (2 cm), the dose was similar for all systems, but this changed with thickness.
"As breast thickness increases, doses vary a lot more, and they increase substantially," Berns said.
The Siemens system had the lowest dose at 2-cm breast thickness but the highest dose at 8-cm thickness, he said.
The Lorad system appears to have a linear dose line across the four levels of breast thickness, Berns said. There were also slight differences between the two systems made by GE, the 2000D and the DS.
At the 2-cm thickness, Lorad had the highest dose. At 8 cm, GE DS had the lowest dose (1.71 mGy), while Siemens' high was 4.43 mGy.
On the ACR phantom images, the GE DS had the lowest dose, while the Lorad system had the highest.
Image quality tests on contrast detail phantoms also revealed big differences. Lorad's Selenia had the highest overall quality score. Siemens' Novation scored lower when breast thickness was lower and better in cases of intermediate thickness.
Significant variations in dosage and quality are due in part to differences in the preprogrammed or recommended techniques, according to Berns.
"In addition to all the clinical technique factors, detector calibration and image processing also play a large part in how images are finally displayed. These two factors affect the end result of the clinical image," Berns said. "Further studies are under way to optimize image quality and dose in digital mammography, with and without automatic exposure modes, to determine if what vendors programmed into your digital mammography systems is what it should be."
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.














