PET/CT Effective Measures NSCLC Biomarker, Predicts Therapy Response
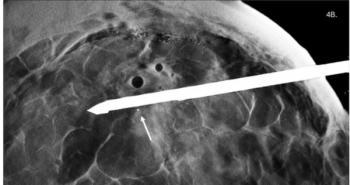
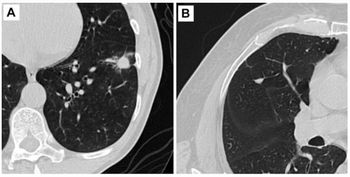
Using PET/CT images to assess the level of a non-small cell lung cancer biomarker can help patients avoid invasive biopsy.
PET/CT images can non-invasively measure levels of a non-small cell lung cancer (NSCLC) biomarker, eliminating the need for biopsy and predicting the patient’s response to therapy.
Checkpoint inhibitors that target the PD1/PD-L1 signaling pathway are an effective treatment for NSCLC, but it only works in roughly half of patients. Investigators from Moffitt Cancer Center demonstrated, in a study published this week in the
“This study is important, as it is the single largest multi-institutional radiomic study population of NSCLC patients to date treated with immunotherapy to predict PD-L1 status and subsequent treatment response using PET/CT scans,” said Robert Gillies, Ph.D., chair of Moffitt’s cancer physiology department. “Because images are routinely obtained and are not subject to sampling bias per se, we propose that the individualized risk assessment information provided by these analyses may be useful as a future clinical decision support tool pending larger prospective trials.”
For their study, the team examined PET/CT scans for nearly 700 patients who had NSCLC who were treated in three institutions. They assessed shape, size, pixel intensity, and textures to train a deep learning tool to accurately measure PD-L1 expression. Using the data, they developed a deep learning score that could predict PD-L1 expression which, after validation, could predict checkpoint inhibitor outcomes in these patients.
Their results point to the usefulness of using images as a replacement for biopsy, said Matthew Schabath, Ph.D., associate member of the cancer epidemiology department.
“These data demonstrate the feasibility of using an alternative non-invasive approach to predict expression of PD-L1,” he said. “This approach could help physicians determine optimum treatment strategies for their patients, especially when tissue samples are not available or when common testing approaches for PD-L1 fail.”
For more coverage based on industry expert insights and research, subscribe to the Diagnostic Imaging e-Newsletter
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.