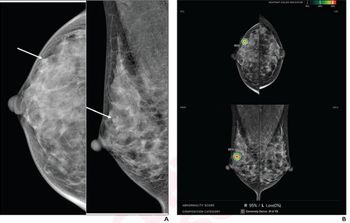
In light of new research showing a 1.6 percent upstaging rate for digital breast tomosynthesis (DBT)-detected radial scars without atypia via core needle biopsy (CNB) findings, the authors of the study maintained that imaging surveillance is the preferred choice over surgery.
For the retrospective study, recently published in the American Journal of Roentgenology, the researchers reviewed data for 153 women (mean age of 56) who had a total of 159 radial scars that were diagnosed with screening DBT. The cohort included 73 patients who had a family history of breast cancer (47.7 percent) and 12 patients who had a prior breast cancer diagnosis (7.8 percent), according to the study.
The study authors found that eight out of 159 radial scars (5 percent) were upstaged to ductal carcinoma in situ (DCIS) or invasive cancer. Out of 129 radial scars without atypia, there were only two cases of upstaging to cancer (1.6 percent). Out of 30 radial scars with atypia, five cases involved upstaging to cancer and one case led to upstaging with invasive disease.
In terms of mammographic findings, the researchers pointed out that six out of the eight cases of upstaging (75 percent) had architectural distortion. They also found no upstaging in 34 cases of radial scars that involved calcifications.
“These findings suggest that surveillance is a reasonable management strategy for radial scars without atypia at CNB, especially when presenting as calcifications,” wrote study co-author Manisha Bahl, M.D., an associate professor at Harvard Medical School and radiologist affiliated with Massachusetts General Hospital in Boston, and Claire Crowley, MB BCh BAO, MSc, a breast imaging fellow at Massachusetts General Hospital.
Three Key Takeaways
- Surveillance over surgery. The study suggests that for radial scars without atypia detected via digital breast tomosynthesis (DBT) and confirmed through core needle biopsy (CNB), surveillance is preferable to surgery as the initial management approach. This approach is especially reasonable when radial scars present as calcifications.
- Risk factors for upstaging. Women with a prior diagnosis of breast cancer are at a significantly higher risk for upstaging of radial scars to cancer. Similarly, radial scars with associated atypia have a substantially greater risk for upstaging. Clinicians should be aware of these factors when deciding between surgical excision and surveillance.
- Imaging characteristics. Architectural distortion was a prevalent mammographic finding in cases where radial scars were upstaged to cancer. Conversely, no upstaging was observed in cases where radial scars involved calcifications. Understanding these imaging characteristics can aid in risk stratification and decision-making regarding management strategies.
In a multivariable analysis, the researchers pointed out that radial scars for women with a prior diagnosis of breast cancer have a 16.85-fold higher risk for upstaging to cancer. They also found that radial scars with associated atypia had a greater than eightfold higher risk for upstaging to cancer.
“Awareness of these factors can help inform clinical management with regard to surgical excision versus surveillance,” added Bahl and Crowley.
(Editor’s note: For related content, see “Five Insights on Artifacts and Limitations with Contrast-Enhanced Mammography,” “Study Shows Benefits of Annual Mammography Exams from 40 to 79 Years of Age” and “Moving Beyond Mammography for Screening and Staging of Invasive Lobular Carcinoma.”)
Beyond the inherent limitations of a single-center retrospective study, the researchers noted there was no assessment of the extent of radial scar removal upon biopsy and 19.5 percent of the cohort did not have a surgical excision procedure. Given that the cohort was comprised of asymptomatic women with radial scars detected during mammography screening, the study authors acknowledged the study findings may not apply for women with symptomatic radial scars.