IR urges moratorium on vertebral compression fracture interventions
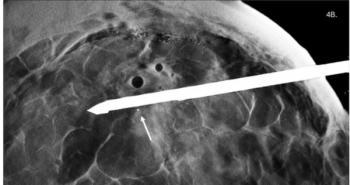
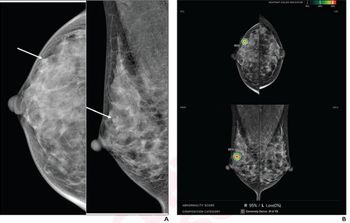
Interventional radiologists should refrain from performing either kyphoplasty or vertebroplasty unless the procedure, intended mostly for the management of pain from vertebral compression fractures, is done in the context of clinical trials.
Interventional radiologists should refrain from performing either kyphoplasty or vertebroplasty unless the procedure, intended mostly for the management of pain from vertebral compression fractures, is done in the context of clinical trials.
Dr. David F. Kallmes, an interventional radiologist at the Mayo Clinic in Rochester, MN, came to this conclusion after analyzing reams of data that nonetheless have been deemed inconclusive. The clinical practice should resume only after results from large, prospective, multicenter trials prove benefits from one or both procedures.
Kallmes was the keynote speaker at a musculoskeletal session at the 2009 RSNA meeting.
“The one thing we learned that is more important than anything else is that we don’t know what we are doing,” Kallmes said.
Recollecting his own experience, Kallmes acknowledged having published several papers on the subject that were “inherently very weak.” Self-criticism aside, he held the whole interventional community accountable for failing to scrutinize research on vertebral stabilization.
“I published pretty bad papers, but they were never criticized. The methods were never questioned, and people accepted them as excellent work,” he said.
The comments also came in the context of two placebo-controlled studies: one by Kallmes, published in the August issue of the New England Journal of Medicine (Investigational Vertebroplasty Efficacy and Safety Trial, INVEST), and the Australian Vertebroplasty trial. Both found vertebroplasty no better than a procedure that simulated vertebroplasty but lacked the bone filler material.
According to Kallmes, INVEST researchers were keen on probing vertebroplasty’s outcomes compared with those of the sham procedure, particularly in regards to pain reduction. But they found no statistically significant differences between them.
The findings were in stark contrast to previous research, which often tended to overstate the positive effects of kyphoplasty and vertebroplasty procedures. Many new questions have been raised, which strongly suggests that investigators, as well as providers, need to plan the future around more trials, Kallmes said.
Members of the audience fervently questioned Kallmes’ data, which came as no surprise. He acknowledged frequent receipt of correspondence from many physicians who have had a hard time accepting and digesting his findings. Most of their accounts, however, reflect only anecdotal experience, he said.
“The successful outcomes we have seen outside clinical trials are simply anecdotes. It is not evidence,” he said.
Despite the controversy fueled by the INVEST and the Australian trials, which have flaws and limitations of their own, their conclusions should not be dismissed, Kallmes said. Both have shed valuable light on the clinical questions that need answering before the minimally invasive repair of vertebral compression fractures becomes an established practice, Kallmes said.
“Practitioners are in an ideal position to advance the field if-and only if-they enroll their patients into clinical trials,” he said.
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.