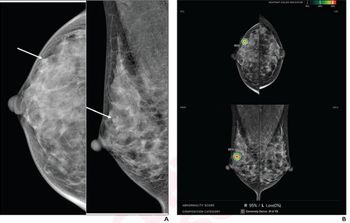
A Good Habit: Consecutive Screening Mammograms Drop Breast Cancer Mortality by Half
Women who do not miss their screening mammography appointments are far less likely to die from breast cancer than women who either forego one – or all – exams.
Skipping an appointment for a screening mammography – even for one year – can put a woman at significantly higher risk for dying from breast cancer. A new study shows that, for women who come in for their routine exams, that risk drops by half.
In a study published in Radiology on March 2, a multi-national team of investigators showed that, based on an observational study of more than half a million women, keeping up with scheduled mammograms can go a long way toward preventing an avoidable death.
“Regular participation in all scheduled screens confers the greatest reduction in your risk of dying from best cancer,” said lead study author Stephen W. Duffy, M.Sc., professor of cancer screening at Queen Mary University of London. “While we suspected that regular participation would confer a reduction greater than that with irregular participation, I think it is fair to say that we were slightly surprised by the size of the effect.”
Related Content:
Even though screening mammography is widely heralded as the best line of defense in catching breast cancers and reducing mortality, a significant number of women still avoid the exam. According to 2018 data from the Centers for Disease Control & Prevention, only 65.3 percent of women in the United States over age 40 go in for routine screening mammograms. The findings from this study, Duffy said, underscore the importance of these exams in helping to stop cancer before it has a chance to grow.
“Missing even one screening examination confers a significant increase in risk,” he said. “This is an important message for women in the screening age groups, their referring physicians, and public health decision makers.”
For their study, the team, led by László Tabár, M.D., professor of radiology at Falun Central Hospital in Sweden, analyzed screening mammography rates for 549,091 women from nine Swedish counties. During the study period from 1992 to 2016, Swedish policy offered women between ages 40 and 54 mammography screening every 18 months; the policy for women between ages 55 and 69 was screening every 24 months.
Related Content:
The women enrolled in the study averaged 58.9 years, and they were divided into four groups. The team categorized them as: serial participants who underwent two consecutive screenings (392,135 women), intermittent participants who had their last – but not next-to-last mammogram (41,746 women), lapsed participants who had their next-to-last – but not most previous – mammogram (30,945 women), and non-serial participants who had neither scheduled exam (84,265 women).
The team identified 3,995 breast cancer deaths across the four groups. Based on their analysis, serial participants had much better outcomes than women who passed by both screening mammograms. Not only did serial participants have a 49 percent lower risk of breast cancer mortality, the team said, but they also 50 percent less likely to die from breast cancer within 10 years. The intermitted and lapsed groups also saw risk reductions of 33 percent and 28 percent, respectively.
When looking at the 2,589 breast cancers that proved fatal within a decade, the 50-percent reduction among serial screeners outpaced the small drops for women in the intermittent and lapsed groups. Those women experienced a 36 percent and 25 percent decrease, respectively.
After adjusting for potential self-selection bias and lead time, the team said, they calculated breast cancer incidence reductions for disease fatal at 10 years. The relative risks were: 0.56 for serial participants, 0.71 for intermittent participants, and 0.81 for lapsed participants.
While these findings do shed light on the benefit provided by screening mammography, the team said they are continuing their work to better understand how the exam affects the interval cancers that pop up in between screenings.
“We are planning further prognostic research into the mechanism of this effect,” Duffy said. “For example, we plan to investigate whether and – if so – to what extent regular attendance improves the prognosis of interval cancers, as well as screen-detected cancers. Estimation of this by time since last screen may have implications for policy on screening frequency.”
For more coverage based on industry expert insights and research, subscribe to the Diagnostic Imaging e-Newsletter
Newsletter
Stay at the forefront of radiology with the Diagnostic Imaging newsletter, delivering the latest news, clinical insights, and imaging advancements for today’s radiologists.